BRAIN and SPINE TUMOURS:
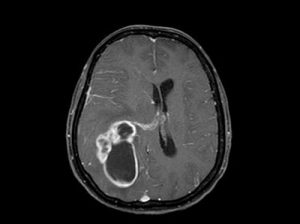
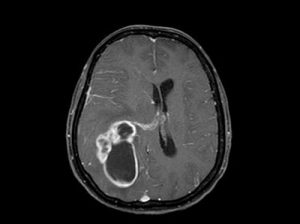
Tumours of the brain, its covering structures and spinal cord can be broadly divided into 2 groups: benign and malignant tumours. Primary brain tumours originate in the brain itself or in tissues close to it, such as in the brain-covering membranes (meninges), cranial nerves, pituitary gland. In contrast a metastatic or secondary tumour spreads to the brain from another part of the body. Primary brain tumours occur in around 250,000 people a year globally, making up less than 2% of cancers. The most common tumour of the brain is a metastatic tumour (figure metastasis) which has spread to the brain from a tumour location in some other part of the body; the commonest being lung cancer.The incidence of metastatic tumors are more prevalent than primary tumors by 4:1
Brain tumours in children can be low grade tumours like pilocytic astrocytomas or high grade developmental tumours like medulloblastomas.
The most common primary brain tumors are:
Gliomas (50.4%)
- The tumor arises from star-shaped glial cells called astrocytes. Glial cells are supporting cells located around neurons. Range from a low grade pilocytic astrocytoma to the malignant glioblastoma multiformae (GBM).

Low grade glioma
Glioblastoma multiformae
Meningiomas (20.8%)
- the tumour arises in the meninges-the covering structure of the brain and spinal cord. (figure meningioma)
Pituitary adenomas(15%)
Nerve sheath tumors (8%)
Nerve sheath tumors (8%) which occur on cranial nerves.
Oligodendrogliomas (4%):
The tumor arises from cells that make the protective substance around nerves. It usually occurs in the cerebrum. It’s most common in middle-aged adults.

Metastatic tumour
Among children the common tumours are:
-
-
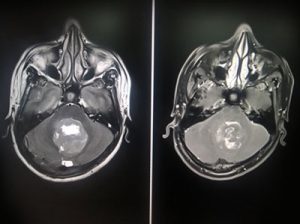
Medulloblastoma (figure Medulloblastoma):
The tumor usually arises in the cerebellum, in the posterior part of the brain. It is a high grade tumour
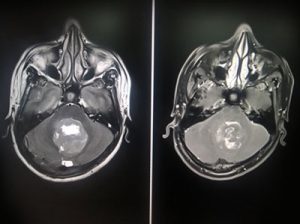
Medulloblastoma
-
-
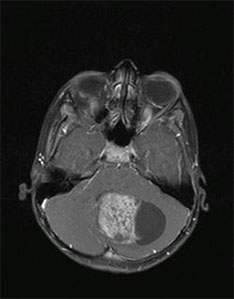
Grade I or II astrocytoma (figure Pilocytic astrocytoma):
In children, this low- grade tumor occurs anywhere in the brain. The most common astrocytoma among children is juvenile pilocytic astrocytoma
Pilocytic astrocytoma
-
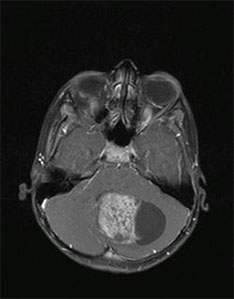
Ependymoma (figure ependymoma):
The tumor arises from cells that line the fluid filled spaces in the brain and spinal cord. It’s most commonly found in children and young adults.

Ependymoma
-
Brain stem glioma:
The tumor occurs in the lowest part of the brain. It can be a low-grade or high-grade tumor.
Causes of brain tumours:
Primary brain tumors begin when normal cells acquire errors (mutations) in their DNA. Tumours are also known to occur in those with genetic syndromes like Neurofibromatosis 1 &2, tuberose sclerosis, Turcot syndrome, Von Hippel Lindau syndrome to name a few. Uncommon risk factors include exposure to vinyl chloride, Epstein–Barr virus, JC virus and ionizing radiation.Only a small percentage of brain tumours run in families.
The symptoms depend on the location, size, and rate of growth of the tumour. Common symptoms include:
- New onset or change in pattern of headaches or headaches that gradually become more frequent and more severe
- Unexplained nausea or vomiting, more towards early morning
- Vision problems, such as blurred vision, double vision or loss of peripheral vision- commonly seen with pitui-tary tumours, but can also be seen in tumours causing raised pressure or along the visual pathway.
- Gradual loss of sensation or movement in an arm or a leg
- Imbalance
- Speech difficulties
- Personality or behavioural changes
- Seizures (fits), especially in someone who doesn't have a history of seizures
- Hearing problems- associated with the eight cranial nerve tumour.
Tumours located in non-critical areas of the brain may continue to grow for an extended period to attain large sizes before they are diagnosed
Classification and grading system: Brain tumours are classified per the World Health Organisation(WHO) Classification of Tumours of the Central Nervous System, last modified in 2016.
Grading system:Brain tumours are graded from I to IV.Cells from low-grade tumors (figure Low grade glioma)(grades I and II) look more normal and generally grow more slowly than cells from high-grade tumors (figure glioblas-toma) (grades III and IV).Over time, a low-grade tumor may become a high grade tumor.
Diagnosis:
Evaluation begins with a complete clinical & neurological examination. For a high suspicion of a brain tumour, MRI is the investigation of choice.MRI can identify early or small tumours missed on CT. Different sequences can define changes in brain tissue and also characterise the tumour itself.MRI can also be used to guide biopsies or resections, as well as in follow-up imaging. Special sequences in MRI like functional MRI and MR tractog-raphy can help locate important areas within the brain and its relation to the tumour. MR spectroscopy helps in indirectly quantifying the grade of the tumour.
CT scan is usually the first-line investigation in emergency presentations. It helps in fast detection of bleed, raised fluid collection within the skull(hydrocephalus) and involvement of bone by tumour.
Hormonal evaluation: Used in pre-operative preparation of pituitary adenomas.
A PET scan would be helpful in the work-up for a metastatic brain tumour in localising the primary and other sites of tumour.
Management :
The choice of treatment depends on:
- The type and possible grade of brain tumour
- Its location in the brain
- Its size
- The persons general health
The 3 modalities for management of brain tumours are surgery, radiation therapy and chemotherapy. Each of these modalities can be used in conjunction with the other based on the grade of tumour, the extent of resection and tumour type.
- Surgery: Surgery is the usual first treatment for most brain tumors. Tumour excision for benign brain tumours and tumour decompression for high grade tumours are usually performed under general anaesthesia. Awake tu-mour surgery is performed under controlled conditions with sedation for tumours located at functionally im-portant regions in the brain. Surgery to open the skull is called a craniotomy, through which the tumour is ap-proached after opening the covering brain structures. After the tumor is removed, the surgeon covers the open-ing in the skull with the piece of bone or with a piece of biocompatible metal or fabric. The surgeon then clos-es the incision in the scalp. Though maximum tumour removal is the goal, the amount of tumour removed de-pends on its location and relation to eloquent areas of the brain. Computer guided tumour removal (neuronavigation ) or stereotactic neurosurgery using MR or CT scan images can precisely localise the tumour in real time and help in tumour removal.
The tumour tissue is then sent for histopathology examination. Special stains including immunohistochemical examination of tumour tissue help characterise the cell of tumour origin. Nuclear indices are defined to grade the aggressiveness of the tumour.
- Radiation therapy: Radiation therapy kills brain tumor cells with high- energy x-rays, gamma rays, or protons.It usu-ally follows surgery for high grade tumours and residual low grade tumours. Highly focused stereotactic radia-tion therapy for well defined tumours of around 2.5 cm in a single sitting has revolutionised management of both primary and metastatic brain tumours.
- Chemotherapy for malignant brain tumours is based on the tissue histology and grade of tumour. It is administered orally or intravenously. For some adults with high-grade glioma, the surgeon may implant several wafers with the chemotherapeutic agent onto the brain at the site of tumour removal. Over a period of time the wafer dis-solves, releasing the agent in the operative area and help prevent tumour from recurring after surgery.
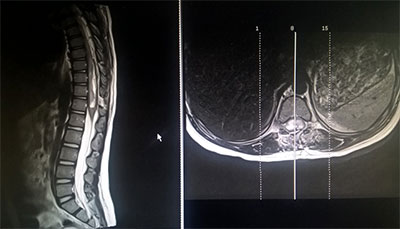
Spinal tumours:
A spinal tumour is a growth that develops within the spinal canal or within the spinal bones. Tumours that arise from the bones of the spine are called vertebral tumours.
A spinal tumor may arise within the spinal cord- most common tumours are astrocytomas or ependymomas (figure spinal intramedullary).
Tumours may also develop from the supporting cells which line the spinal cord or spinal nerves. Most common tumours are schwannomas, meningiomas and neurofibromas. Though the lie outside the spinal cord, they can compress the spinal cord and produce symptoms.
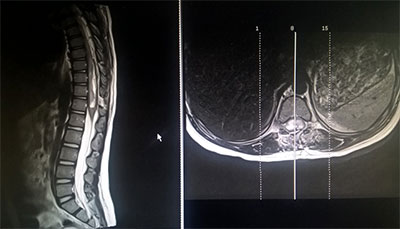
Spinal intramedullary ependymoma
Spinal intramedullary ependymoma
Common symptoms of spinal tumours are: back pain, difficulty in using hands or walking, altered sensation in hand or legs, bowel and bladder disturbances.
Diagnosis: MRI is the modality of choice for evaluation of spinal tumours. It provides information on the location of tumour, its relation to the spinal cord and nerves.
Management:
Surgery for spinal tumours provides tissue for histopathological examination. Adjuvant therapy in the form of radiation for tumours like astrocytomas and ependymomas is based on tissue biopsy and extent of surgical resection. For tumours like meningiomas and neurofibromas/schwannomas complete excision forms the mainstay of treatment.
Spine tumor spine specimen


 Low grade glioma
Low grade glioma
 Glioblastoma multiformae
Glioblastoma multiformae